Fibrodysplasia Stoneman Syndrome: Ossificans Progressiva
Why is Stoneman syndrome called that?
It has also been referred to as “Stone Man Disease” because it results in painful, stony-hard swellings that are severely morbid and disabling. In the medical literature, only roughly 600 cases have been described.
How long is Stoneman syndrome tolerable?
The average lifespan is about 40 years old. By the second decade of life, the majority of patients are wheelchair-bound and frequently pass away from thoracic insufficiency syndrome-related problems.
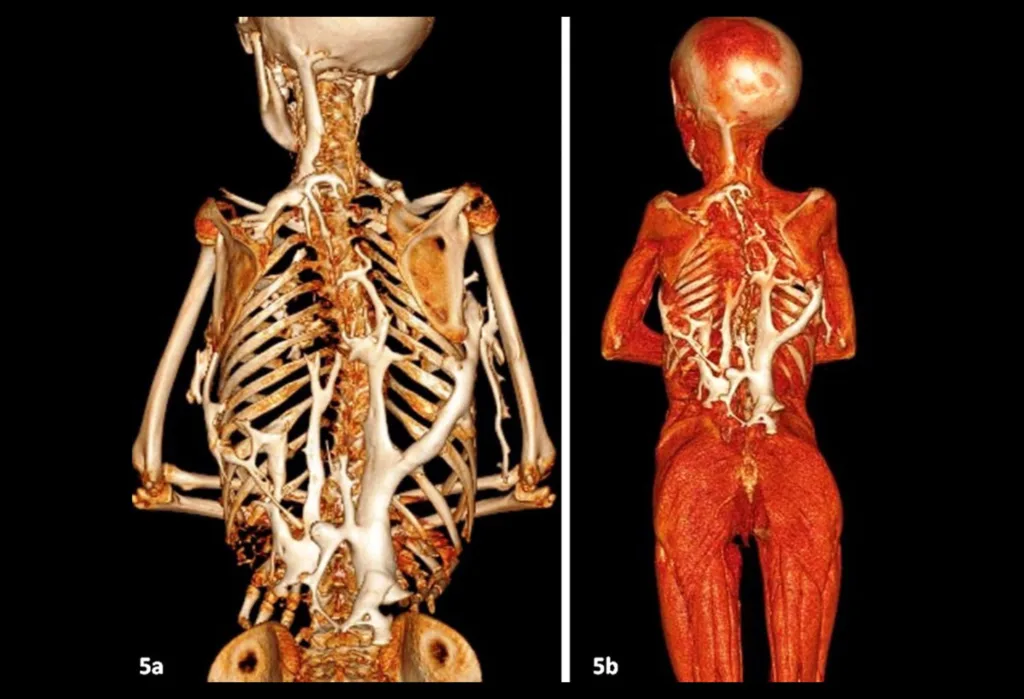
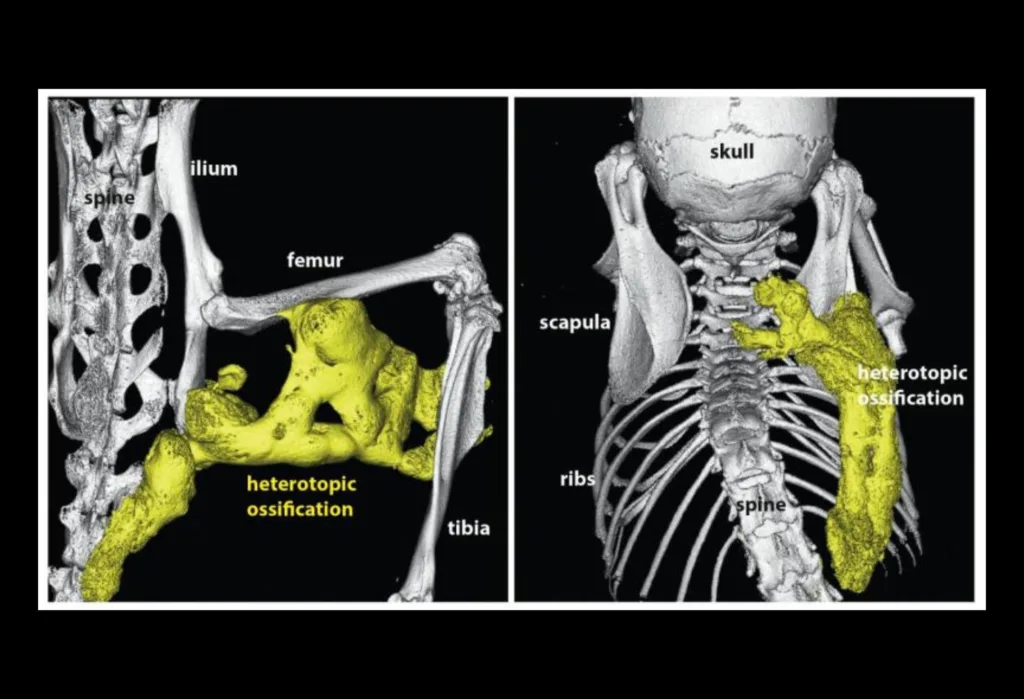
A condition known as fibrodysplasia ossificans progressiva causes the bone to gradually replace muscle and connective tissue, such as tendons and ligaments, resulting in the extra-skeletal or heterotopic bone that restricts motion. This process, which begins in the neck and shoulders and moves down the body and into the limbs, usually becomes apparent in early childhood.
As the joints are impacted by extra-skeletal bone development, there is a progressive loss of motion. Speaking and eating may be challenging if one’s mouth won’t fully open. People with this disorder may eventually become malnourished due to their eating issues. In addition, they can suffer breathing problems if additional bone growth around the rib cage prevents the lungs from expanding fully.
A fall or invasive medical procedures may cause periods of muscle swelling and inflammation (myositis), which are then followed by more rapid ossification in the wounded area in a person with fibrodysplasia ossificans progressiva. Viral infections like the flu can also bring on flare-ups.
Most fibrodysplasia ossificans progressiva patients have deformed big toes at birth. This condition can be distinguished from other bone and muscular issues because of the abnormalities of the big toes. Other bone anomalies, including short thumbs, are possible in those who are affected.
Is there a cure for Stone Man Syndrome?
FOP is a rare and incapacitating condition for which there is no cure or viable treatment that can halt its progression. The main focus should be on educating medical professionals, surgeons, patients, and their families about the illness. Families should also receive the appropriate counseling.
What happens when the muscle becomes bone?
A condition known as fibrodysplasia ossificans progressiva causes the bone to gradually replace muscle and connective tissue, such as tendons and ligaments, resulting in the extra-skeletal or heterotopic bone that restricts motion.
Can bones become solid rock?
By means of a process known as petrification, a very detailed fossil is created. This occurs when groundwater switches out bone or wood for minerals like silica. Over the course of millions of years, the cells of the bone or wood are gradually replaced, one molecule at a time.
Can those who have FOP (Fibrodysplasia Ossificans Progressiva)become parents?
Due to the absence of involvement of the smooth muscles in this syndrome, pregnancy is a rare occurrence in FOP; yet, at least five known occurrences of births have been documented in the medical literature, including two in this study.
Does FOP (Fibrodysplasia Ossificans Progressiva)hurt?
FOP could finally cause total immobility. People who are affected may have progressive pain and stiffness in the affected areas, full spinal fusion, or pain from aberrant bone growths that push on the nerves in these places (entrapment neuropathies).

Causes
Fibrodysplasia ossificans progressiva is caused by variations (sometimes referred to as mutations) in the ACVR1 gene. Bone morphogenetic protein (BMP) type I receptors are made using the instructions provided by this gene. Skeletal muscle and cartilage are two bodily tissues that contain the ACVR1 protein.
It aids in regulating bone and muscle growth and development, including the gradual replacement of cartilage by bone (ossification) that takes place during typical skeletal maturation from birth to adolescence.
According to studies, the ACVR1 gene’s variations mess with the mechanisms that regulate the function of the receptor. As a result, the receptor is activated when it ought to be off. The signs and symptoms of fibrodysplasia ossificans progressiva are brought on by excessive receptor activation, which leads to the expansion of bone and cartilage.
Alternative Names for This Illness
• Ossific myositis
• FOP (Fibrodysplasia Ossificans Progressiva)
• Myositis progressive ossificans
• Ossificative progressive myositis
• Progression of osseous myositis
What signs indicate Stoneman Syndrome?
The genetic condition is both simple to identify and challenging to diagnose because of its nature. Due to its rarity and low level of public awareness, FOP is sometimes mistaken for less serious forms of other muscular illnesses. On the other hand, it is simple to diagnose due to its specific symptoms. This rare genetic illness will likely pass to your offspring if you or a family member has it.
One can observe it by closely examining their newborn child’s toes and thumbs. The big toes and, in rare circumstances, the thumbs of newborns with this disease are deformed at birth.
In addition, kids with Stoneman Syndrome may exhibit any of the following symptoms as they mature:
• Limited joint movement, particularly at first in the neck and shoulders.
• An abnormal spine.
• Frequently feeling unbalanced while moving, which is followed by joint pain, inflammation, and a low-grade fever.
•Surface reflection of the body’s aberrant bone growth ( except the tongue, diaphragm, extraocular muscles, cardiac muscle, and smooth muscle).
• Difficulty speaking, breathing, or eating.
• Unhealthy hearing ( rare).
• An obvious enlargement of the afflicted area.
As the child ages, these symptoms will worsen as the body’s tissues begin to ossify not only in the upper part of the body but also in the trunk, back, hips, and limbs, eventually rendering the person fully immobile.
What therapies are available to treat Stoneman Syndrome?
Since there is currently no effective treatment for genetic conditions like fibrodysplasia ossificans progressiva, and since removing the bone will merely encourage the creation of new, more painful heterotopic bone, doctors have developed a few drugs that lessen the rate and severity of ossification:
• High doses of corticosteroids, such as Prednisone, to treat early-stage pain and swelling flare-ups. Before administering nonsteroidal anti-inflammatory medicines (NSAIDs), which must be taken in between flare-ups.
• Relaxants for muscles.
• Mast cell blockers.
• Aminobisphosphonates.
• Occupational therapy;
• Assistive devices, such as braces or special shoes to aid in walking
Things that can accelerate ossification and cause physical discomfort are among the things that must be watched over the course of treatment.
Treatments and diagnoses involving bone, such as biopsy, intramuscular injections (immunizations), and bending the jaw during dental operations, need to be avoided since they can harm the skeletal system and exacerbate the ossification process in the affected area.
A flare-up in the heterotopic bone can be caused by blunt trauma or injury, so it’s important to avoid getting wounded. Any physical activity that increases the danger of falling or receiving other injuries needs to be limited.
For two main reasons, it is advised to postpone having children if you have FOP. First, your genetic dysfunction could be passed on to your offspring, making it difficult for them to survive for the rest of their life. Second, as the foetus grows inside the womb, the chance of flare-ups, which can be fatal for both mother and child, increases.
How is Stoneman Syndrome medically diagnosed?
A rare genetic disease diagnosis can be difficult. FOP instances can initially be mistaken for other muscularly aggressive conditions such as juvenile fibromatosis, malignancy, and fibrous dysplasia. Malformed big toes are the only symptom that distinguishes it from other disorders.
Your healthcare provider will review your medical and family history to check for any genetic patterns, just like with any other medical diagnosis, and then conduct a number of physical exams and laboratory tests. A genetic testing registry and imaging tests like X-rays and MRIs could be part of your laboratory test (GTR).
While GTR will give the doctor guidance in selecting the best genetic tests for this problem, imaging tests will assist the doctor in observing the heterotopic bone’s overall progress. A team of medical experts who specialize in researching and analyzing such uncommon disorders undertakes GTR, which involves asking both the patient and the medical staff a number of questions.
Conclusion
FOP is a rare and incapacitating condition for which there is no cure or viable treatment that can halt its progression. The main focus should be educating doctors, surgeons, patients, and their families about the illness. Families should also receive the right therapy.
The best course of action is still seen to be early diagnosis and injury avoidance for patients to assist them avoid flare-ups; nonetheless, symptomatic therapy with medications is indicated. Till heterotopic ossifications are fully ripe and surgery is clearly warranted, surgeons should wait to remove them.

