Uveitis is a term that is used to describe a variety of disorders that result in inflammation of the centre layer of the eye, known as the uvea, as well as the tissue that surrounds it. It may cause pain, the affected eye or eyes may become inflamed, and haziness may appear in the affected field of vision.
Uveitis can be brought on by a number of factors, including trauma to the eye, an infection caused by bacteria or viruses, and even some preexisting conditions. It has the potential to enlarge the tissue of the eye and cause harm to that tissue. If it is not addressed, it might result in vision loss as well as other problems. It could harm either eye or both of them.
An inflammation that affects the uvea as well as any other component of the eye’s interior is referred to as uveitis. There are numerous subtypes of uveitis, each of which may have a unique underlying aetiology.
People between the ages of 20 and 60 are most likely to be affected. Trusted Source, although the illness can affect people of any age or background.
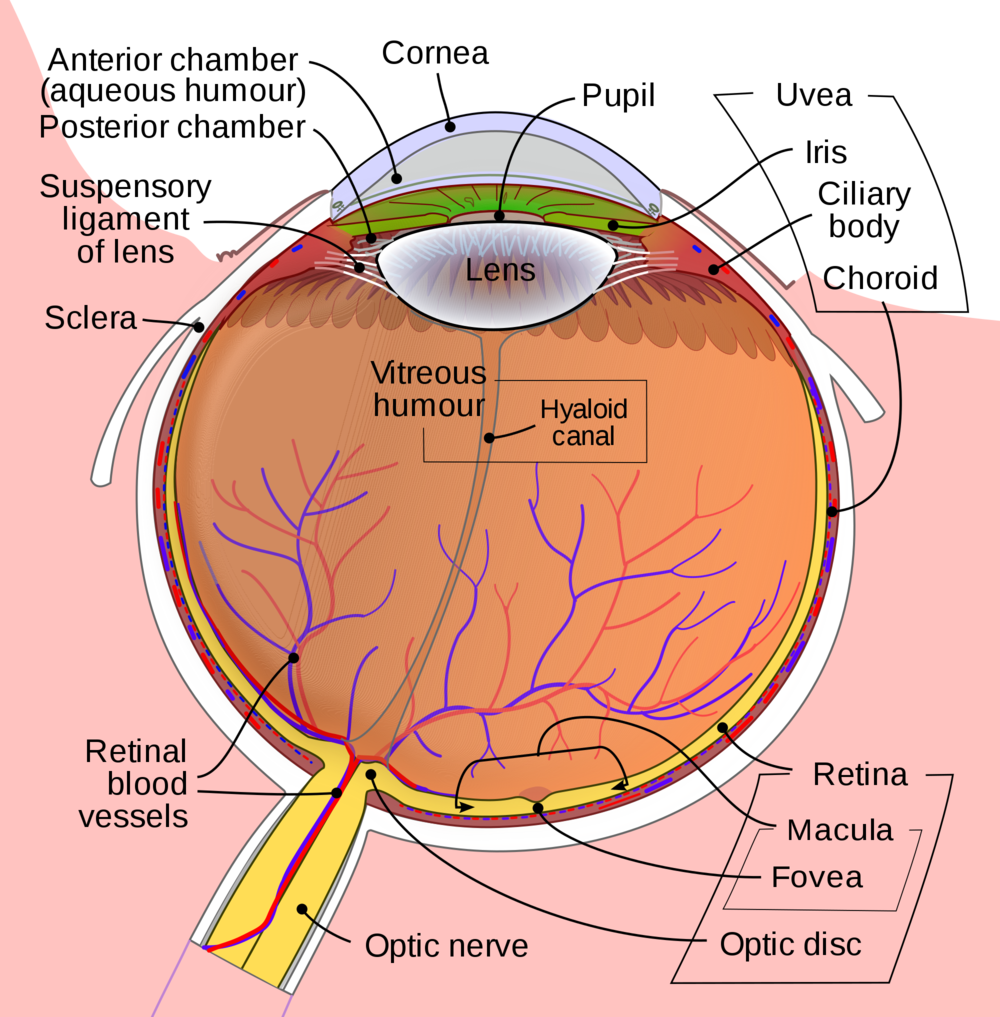
The uvea is the layer of the eye that may be found in the centre of the retina and the sclera (the white area of the eye) (the light-sensitive layer at the back of the eye). There are three components to it:
*Iris (the coloured part of the eye)
*Ciliary body (the part of the eye that helps the lens focus)
*Choroid (the part of the eye that connects the retina to the sclera)
Which kind of uveitis are there to choose from?
Various forms of uveitis cause inflammation in a variety of regions of the eye. The iris at the front of the eye is affected when you have anterior uveitis. It is the most prevalent form, and it typically does not do as much damage.
In patients with intermediate uveitis, both the ciliary body and the vitreous are affected (the gel-like fluid that fills the eye).
At the back of the eye, where the retina and the choroid are located, posterior uveitis causes inflammation.
Panuveitis is an inflammation that can affect any and all portions of the uvea, from the cornea to the retina.
What signs and symptoms are associated with uveitis?
Symptoms of early uveitis typically manifest all of a sudden. Among the symptoms are:
*Vision that is hazy.
*Floaters (small dark spots or squiggly lines that float across your vision)
*Eye pain
*Oculi rossi
*sensitivity to the effects of light
Visit an eye doctor as soon as possible if you observe any of these symptoms. If the condition is not treated, uveitis might result in vision loss.
Types
According to the location of the uvea where the inflammation first manifests, there are four distinct forms of uveitis. A person must first be familiar with the uvea in order to comprehend the various categories of this structure.
What exactly is a uvea?
The uvea is the layer of tissue that may be found in the middle of the wall of the eye. It is also known as the uveal layer, the uveal coat, the uveal tract, and the vascular tunic. This layer located within the eye contributes to multiple tasks, including the absorption of light and the focussing of the retina.
The uvea is made up of a few different sections. Among these are the following:
iris, also known as the colourful region of the eye that surrounds the pupil choroid, which assists the lens in focusing on objects in its field of view
the ciliary body, also known as the ciliary ring, is a ring of muscle that is located behind the eye and connects the retina to the sclera.
As will become clear in the following section, the various kinds of uveitis impact various regions of the uvea.

Anterior uveitis
The most typical presentation of uveitis is known as anterior uveitis. This condition, which affects the cornea of the eye and is also referred to as iritis, is diagnosed by seeing the presence of white blood cells and fibrin in the anterior chamber of the eye (front part of the eye). The iris, it is believed by the medical community, may have been inflamed. Iridocyclitis is a condition that is quite similar to uveitis, but it additionally involves inflammation of the ciliary body.
Intermediate uveitis
There are two subtypes of intermediate uveitis: vitritis and pars planitis. Vitritis is an inflammation of the vitreous cavity, which is the area of the eye that is similar to jelly. Pars planitis is the name given to the condition that occurs when there is no underlying cause for intermediate uveitis.
Posterior uveitis
Inflammation of the choroid and the retina is what is known as posterior uveitis. The posterior region of the eye is often known as the back of the eye.
Panuveitis
Inflammation that affects all layers of the uvea is referred to as panuveitis. This particular form of uveitis has the potential to spread to other parts of the eye, such as the lens, the retina, the optic nerve, and the vitreous. It is possible for it to lead to impaired vision or perhaps blindness.
Uveitis symptoms
Uveitis can present itself with a wide variety of signs and symptoms. The majority of the time, they come on all of a sudden, but they can also develop gradually. Among the possible symptoms are the following:
- pain and redness in the eye floaters, which are spots in the eye that look like tiny rods or chains of transparent bubbles floating around in the field of vision redness and pain in the eye floaters
- issues with vision in general, including haziness or blurriness of vision
- Headaches are a common symptom of photophobia, an excessive sensitivity to light.
- Uveitis has the potential to lead to visual loss if it is not treated.
Uveitis causes
Anyone is at risk of developing uveitis. There is a possibility that the inflammation is localised to the eye, but it could also be associated with bacterial or viral infections, autoimmune illnesses, or damage.
The following infections, among others, may cause uveitis or raise the risk of developing the condition:
- HIV and AIDS epidemic
- The herpes simplex virus
- brucellosis
- shingles
- leptospirosis
- The disease is known as Lyme
- tuberculosis syphilis toxocariasis and other forms of toxoplasmosis syphilis (TB)
Uveitis can be brought on by autoimmune diseases as well as inflammatory conditions. These are the following:
- psoriasis
- arthritis rheumatoid in patients
- an illness known as Crohn’s
- inflammatory bowel disease arthritis ankylosing spondylitis ulcerative colitis
- Vogt-Koyanagi-Harada (VKH) sickness
- multiple sclerosis (MS)
- Uveitis can also be brought on by trauma to the eye, another potential trigger. Trauma or contact with harmful substances can also result in injury.

Diagnosis
When an ophthalmologist examines a patient’s eyes, they will be able to recognise uveitis if it is present.
During the course of an eye exam, an ophthalmologist will most likely examine the patient’s eyes using a device known as a slit lamp. The presence of white blood cells in the anterior chamber or vitreous of the eye is the defining characteristic of uveitis.
In addition to these results, there were lumps on the cornea that were referred to as keratic precipitates. Patients who have inflammation in the iris may experience some pain when the pupil contracts, which occurs when light strikes it. This is because light causes the pupil to constrict.
Because there are a variety of possible underlying disorders that can cause uveitis, an opthalmologist may refer a patient to a rheumatologist or a specialist in uveitis so that the patient can have a comprehensive examination and receive a diagnosis of an underlying ailment.
Treatment
Patients diagnosed with uveitis who receive treatment that is timely and adequate typically make a full recovery. If therapy is not received, there is an increased chance of vision loss that is irreversible, cataracts, glaucoma, band keratopathy, and edoema of the retina.
Corticosteroid drops are the most prevalent form of treatment for uveitis, as stated by the American Academy of Ophthalmology. These drops are used to help reduce inflammation caused by the condition. Additionally, eye medications can be used to help open the pupils, which in turn lessens pain and swelling in the affected area.
An ophthalmologist may also recommend or prescribe one of the following, depending on the patient’s condition:
- steroids that are taken orally in the form of pills steroids that are injected and administered either around or in the eye a surgical implant that releases modest amounts of steroids over the course of time
- To further assist in dampening the reaction of the immune system, a physician might further suggest immunomodulator therapy or biologics.
- If an optometrist has reason to suspect that a patient is suffering from an autoimmune condition, they will most likely suggest that the patient seek out the services of a rheumatologist for more specialist therapy.
The type of uveitis can influence the treatment that a physician prescribes for the condition.
- Managing the symptoms of anterior uveitis
- The following are some of the more prevalent treatments for anterior uveitis:
- drops for the eyes that dilate the pupils and relieve the strain on the eyeballs
- topical corticosteroids
- Uveitis treatment for the intermediate and posterior segments
What kind of medicine is used to treat uveitis?
Steroid medications have been shown to be effective in reducing inflammation in the eye. This can alleviate discomfort and stop eyesight loss from occurring. Steroid medication could be prescribed to you by your ophthalmologist in one of the following ways:
*Eye drops. The most typical therapy consists of using eye drops that are prescribed by a doctor.
*Pills. Your eye doctor could also recommend that you take steroids in oral form.
*Injections. In certain instances, your eye doctor may use a very thin needle to inject the steroid directly into or around your eye.
*Implants. If previous treatments are unsuccessful, your doctor may recommend that you undergo surgery to have a small device known as an implant placed inside of your eye. The steroid will be delivered to your body at regular intervals and in very small dosages thanks to the implant.
*Steroids are known to have a variety of adverse consequences, including an increased likelihood of developing cataracts and glaucoma.If you are prescribed steroids for uveitis, getting routine eye exams to look for warning signals of complications caused by the medication is very important.
Your course of therapy will be determined by a number of factors, such as which area of your eye is affected and any other health concerns you may have. For instance, your physician can recommend that you take certain medications to assist bring your immune system under control. You and your physician can collaborate to identify the treatments that are most effective for you.
When treating intermediate and posterior uveitis, a physician may resort to the following additional treatment methods:
Antivirals, antibiotics, or other medications nonsteroidal anti-inflammatory drugs (NSAIDs) to treat pain and swelling corticosteroids — injections, intravenous, implants, or oral antivirals, or other medications nonsteroidal anti-inflammatory drugs (NSAIDs) to treat inflammation immunosuppressants, corticotropin biologic agents
Complications
The potential for problems can be mitigated by initiating therapy as soon as possible and maintaining continuous monitoring.
In the event that they do take place, some of the following may take place:
- glaucoma
- cataracts
- macular edoema
- scar tissue
- retinal detachment, or detached retina
- vision loss
Determinants of risk
A person’s likelihood of acquiring uveitis is affected by a number of different factors. The following are some common forms of risk:
- the use of certain drugs while smoking
- vitamin D levels having an inflammatory condition such as rheumatoid arthritis being pregnant or planning to become pregnant
- In addition, the risk of getting uveitis is significantly greater in females than it is in males.
Recovery
There are two distinct forms of uveitis: acute and chronic. The subtype a person has can have an impact on how well they recover.
Both acute (lasting only a few weeks) and chronic forms of anterior uveitis are possible (lasting for 3 or more months). The majority of cases of posterior uveitis are chronic, and it normally takes a person several months to make a full recovery after being diagnosed with the condition.
On the other hand, it is not possible to accurately predict how long each individual case will continue. To achieve a successful recovery, a person should discuss their prognosis with their treating physician and adhere to all of the therapy suggestions.
Outlook
In most cases, a person has a constructive point of view. The majority of individuals will not go blind for good. People who live with chronic types of uveitis have a higher risk of developing additional disorders that might lead to vision loss, such as cataracts or glaucoma.
If a person follows all of the treatment recommendations to lessen the pressure and inflammation in their eye, they can lower the likelihood that they will suffer from a visual loss that is permanent.
Prevention
People who live with an underlying ailment, such as rheumatoid arthritis or multiple sclerosis, can aid in the prevention of uveitis by adhering to the treatment programmes that have been laid out for them and remaining in remission from their disease.
Uveitis has no cure. Instead, the treatment focuses on lowering inflammation and swelling in the affected area. However, the condition can be put into remission with the utilisation of immunomodulatory treatment.
In order to address underlying illnesses, such as rheumatoid arthritis or multiple sclerosis, a person might be able to make use of natural or complementary therapy. However, prior to beginning a new treatment, a person should consult with their primary care physician regarding alternative therapies.

What is the key distinction between conjunctivitis and uveitis?
The layer of the eye that is affected by either condition—the conjunctiva for conjunctivitis and the uvea for uveitis—is the primary distinction between the two. Uveitis affects the layer that is located in the middle of the eye, while conjunctivitis, often known as pink eye, affects the outermost layer of the eye.
The reasons can also be different. In contrast to conjunctivitis, which is often brought on by ocular infection caused by bacteria, viruses, or fungi, uveitis can sometimes develop as a consequence of inflammation brought on by an autoimmune condition. There is also the possibility that it was caused by an irritant or allergen going into the eye.
In most cases, vision problems are not associated with conjunctivitis, despite the fact that both conditions can make the eyes red and inflamed. On the other hand, a person may experience discharge, itching or irritation of the eye, watery eyes, and the sensation that something is lodged in the eye.
Takeaway
Uveitis is an inflammation that can damage multiple components of the middle layer of the eye. According to the region of the eye that is affected, uveitis can take on a number of distinct forms. A person’s ability to make a full recovery from an illness depends on whether they develop the acute or chronic form of the illness.
Different treatments may be used, but the primary goal in all of them is to lessen inflammation and swelling so that problems can be avoided. People who live with a secondary condition on top of their primary illness, like MS, should collaborate with their primary care physician to manage both conditions.